1. A 5-year-old child presents with lethargy, increased work of breathing, and pale color. The primary assessment reveals that the airway is open and the respiratory rate is 30/min, with crackles heard on auscultation. The cardiac monitor shows sinus tachycardia at a rate of 165/min. The pulse oximeter displays an oxygen saturation of 95% and a pulse rate of 93/min. On the basis of this informatio
...[Show More]
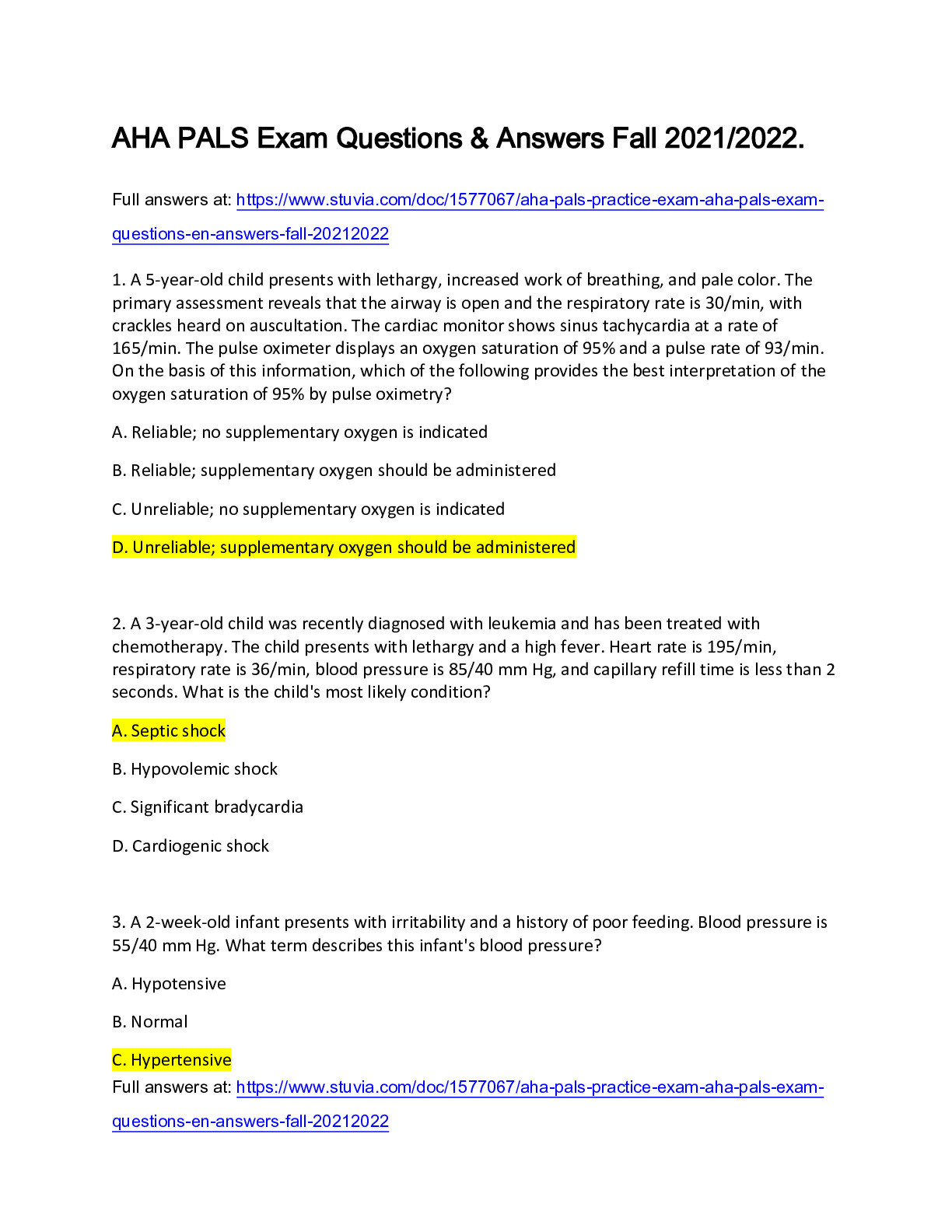
1. A 5-year-old child presents with lethargy, increased work of breathing, and pale color. The primary assessment reveals that the airway is open and the respiratory rate is 30/min, with crackles heard on auscultation. The cardiac monitor shows sinus tachycardia at a rate of 165/min. The pulse oximeter displays an oxygen saturation of 95% and a pulse rate of 93/min. On the basis of this information, which of the following provides the best interpretation of the oxygen saturation of 95% by pulse oximetry?
A. Reliable; no supplementary oxygen is indicated
B. Reliable; supplementary oxygen should be administered
C. Unreliable; no supplementary oxygen is indicated D. Unreliable; supplementary oxygen should be administered
2. A 3-year-old child was recently diagnosed with leukemia and has been treated with chemotherapy. The child presents with lethargy and a high fever. Heart rate is 195/min, respiratory rate is 36/min, blood pressure is 85/40 mm Hg, and capillary refill time is less than 2 seconds. What is the child's most likely condition? A. Septic shock
B. Hypovolemic shock
C. Significant bradycardia
D. Cardiogenic shock
3. A 2-week-old infant presents with irritability and a history of poor feeding. Blood pressure is 55/40 mm Hg. What term describes this infant's blood pressure?
A. Hypotensive
B. Normal
C. Hypertensive
D. Compensated
4. During a resuscitation attempt, the team leader orders an initial dose of epinephrine at 0.1 mg/kg to be given 10. What should the team member do?
A. Administer the drug as ordered
B. Administer 0.01 mg/kg of epinephrine C. Respectfully ask the team leader to clarify the dose
D. Refuse to administer the drug
5. Which of the following is a characteristic of respiratory failure? A. Inadequate oxygenation and/or ventilation
B. Hypotension
C. An increase in serum pH (alkalosis)
D. Abnormal respiratory sounds
6. Which of the following is most likely to produce a prolonged expiratory phase and wheezing?
A. Disordered control of breathing
B. Hypovolemic shock C. Lower airway obstruction
D. Upper airway obstruction
7. A 4-year-old child presents with seizures and irregular respirations. The seizures stopped a few minutes ago. Which of the following most likely to be abnormal?
A. Vascular resistance
B. Pulse rate
C. Lung compliance
D. Control of breathing
8. What abnormality is most likely to be present in children with acute respiratory distress caused by lung tissue disease? A. Decreased oxygen saturation
B. Stridor
C. Normal respiratory rate
D. Decreased respiratory effort
9. An alert 2-year-old child with an increased work of breathing and pink color is being evaluated. Heart rate is 110/min, and respiratory rate is 30/min. What would best describe this patient's condition? A. Respiratory distress
B. Respiratory arrest
C. Respiratory failure
D. Disordered control of breathing
10. The parents of a 7-year-old child who is undergoing chemotherapy report that the child has been febrile and has not been feeling well, with recent onset of lethargy. Assessment reveals the following: The child is difficult to arouse, with pale color. The child's heart rate is 160/min, respiratory rate is 30/min, blood pressure is 76/45 mm Hg, capillary refill time is 5 to 6 seconds, and temperature is 103°F (39.4°C). What is the most appropriate intervention?
A. Obtain vascular access and administer 20 mL/kg of isotonic crystalloid over 30 minutes B. Obtain vascular access and administer 20 mL/kg of isotonic crystalloid over 5 to 10 minutes
C. Obtain immediate blood cultures and chest x-ray D. Obtain expert consultation with an oncologist to determine the chemotherapeutic regimen
11. A 2-year-old child presents with a 4-day history of vomiting. The initial impression reveals an unresponsive child with intermittent apnea and mottled color. Heart rate is 166/min, respiratory rate is now being supported with bag-mask ventilation, capillary refill time is 5 to 6 seconds, and temperature is 102°F (38.9°C). What is the best method of establishing immediate vascular access?
[Show Less]